 Chronic pain and breathing disorders can be effectively treated with various technologies that take the frustration out of treatment for both the clinician and the patient. Check out the variety of technologies that help Dr. Steven Olmos treat these disorders.
Chronic pain and breathing disorders can be effectively treated with various technologies that take the frustration out of treatment for both the clinician and the patient. Check out the variety of technologies that help Dr. Steven Olmos treat these disorders.
Educational aims and objectives: This clinical article aims to discuss how to treat chronic pain and breathing disorders with technology.
Expected outcomes:
 This paper quantifies the reduction of soft tissue hypertrophy of the nasal complex resulting in an increase of nasal volume and increased flow using a mixture of Xylitol and Saline. The health benefits of improved nasal breathing through increased inspired nasal NO (nitric oxide) and the antimicrobial benefits of Xylitol are discussed. Restoration of functional breathing (nasal) and it’s relation-ship to up righting head posture is reviewed. Keywords: Xlear; Xylitol; Nasal Obstruction; Forward Head Posture; Nitric Oxide
This paper quantifies the reduction of soft tissue hypertrophy of the nasal complex resulting in an increase of nasal volume and increased flow using a mixture of Xylitol and Saline. The health benefits of improved nasal breathing through increased inspired nasal NO (nitric oxide) and the antimicrobial benefits of Xylitol are discussed. Restoration of functional breathing (nasal) and it’s relation-ship to up righting head posture is reviewed. Keywords: Xlear; Xylitol; Nasal Obstruction; Forward Head Posture; Nitric Oxide
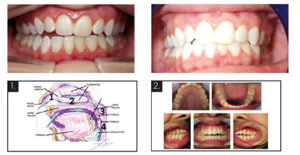
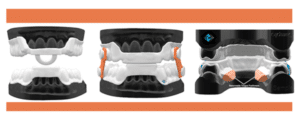 Oral appliances designed for relief of facial pain and jaw dysfunction, sleep breathing disorders, and orthodontics have been utilized for many years with little change in materials until recently. This article will review indications/limitations of existing designs/materials, and how computer-aided manufacturing allows for better and healthier alternatives. There is always a reason for patients’ symptoms. Chronic face, jaw, head, and neck pain are all interrelated and are highly comorbid with sleep breathing disorders.1 Malocclusion, skeletal development deficiencies, and teeth crowding are symptoms of a functional breathing disorder.2-7 Oral appliances are used for each indication.
Oral appliances designed for relief of facial pain and jaw dysfunction, sleep breathing disorders, and orthodontics have been utilized for many years with little change in materials until recently. This article will review indications/limitations of existing designs/materials, and how computer-aided manufacturing allows for better and healthier alternatives. There is always a reason for patients’ symptoms. Chronic face, jaw, head, and neck pain are all interrelated and are highly comorbid with sleep breathing disorders.1 Malocclusion, skeletal development deficiencies, and teeth crowding are symptoms of a functional breathing disorder.2-7 Oral appliances are used for each indication.
 nbcnews.com
nbcnews.com
These tips will help you survive the day when you’re running on empty.
 Orthodontic Practice US (Volume 8 Number 3) | March 2017 A case study featuring a young patient is presented as an example of the airwaycentered philosophy that essentially is defined as a mandibular relationship that produces the optimal orthopedic function of the temporomandibular (TM) joints and prevents or reduces airway collapse (oropharyngeal) in the unconscious state (sleep).
Orthodontic Practice US (Volume 8 Number 3) | March 2017 A case study featuring a young patient is presented as an example of the airwaycentered philosophy that essentially is defined as a mandibular relationship that produces the optimal orthopedic function of the temporomandibular (TM) joints and prevents or reduces airway collapse (oropharyngeal) in the unconscious state (sleep).
 by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO This article defines “Airway Centered Dentistry”, explains the mechanism of chronic face/jaw pain and dysfunction, reviews the technique and triage systems that have been successful in the standardized approach currently utilized in 45 TMJ and Sleep Therapy Centres in seven countries.
by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO This article defines “Airway Centered Dentistry”, explains the mechanism of chronic face/jaw pain and dysfunction, reviews the technique and triage systems that have been successful in the standardized approach currently utilized in 45 TMJ and Sleep Therapy Centres in seven countries.
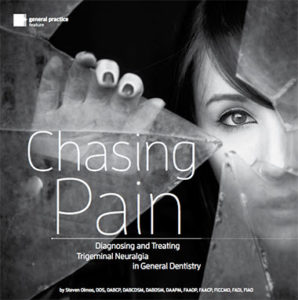 As dentists, we know quite a bit about tooth and gum pain, but when it comes to chronic facial pain and neuropathic pain, our dental school education leaves us unprepared. The objective of this article is to explain the differences between men and women with chronic orofacial pain and the relationship to proper functional breathing.
As dentists, we know quite a bit about tooth and gum pain, but when it comes to chronic facial pain and neuropathic pain, our dental school education leaves us unprepared. The objective of this article is to explain the differences between men and women with chronic orofacial pain and the relationship to proper functional breathing.
 Purpose: To investigate the relationship between craniofacial pain symptoms (painful conditions present in the cranium and face, including jaw joint-related pathology and primary headache conditions) and daytime sleepiness, determined by the Epworth sleepiness scales (ESS), to correlate the comorbidity as well as potential predictive factors.
Purpose: To investigate the relationship between craniofacial pain symptoms (painful conditions present in the cranium and face, including jaw joint-related pathology and primary headache conditions) and daytime sleepiness, determined by the Epworth sleepiness scales (ESS), to correlate the comorbidity as well as potential predictive factors.
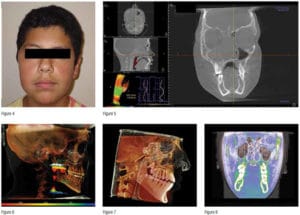
 The purpose of this case study is to demonstrate the relationship between obstructive sleep apnea (OSA), obesity, TMD, and headache in the pediatric population. It is possible to resolve OSA in children whereas we most often only manage it in the adult population. This demonstrates the need to identify the clinical signs and screen for sleep-breathing disorder symptoms in children and adolescents.
The purpose of this case study is to demonstrate the relationship between obstructive sleep apnea (OSA), obesity, TMD, and headache in the pediatric population. It is possible to resolve OSA in children whereas we most often only manage it in the adult population. This demonstrates the need to identify the clinical signs and screen for sleep-breathing disorder symptoms in children and adolescents.
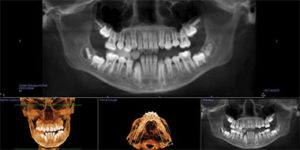 This article seeks to evaluate the 3D volumetric changes that are necessary to treat pediatric Obstructive Sleep Apnea (OSA). Adult static therapies are not indicated for children. Children require dynamic therapies to encourage and correct skeletal development to improve sleep-breathing disorders. Formulas for arch width expansion are currently based on dental space and skeletal calculations and are not applicable nor are they validated in the treatment of pediatric OSA. Treating children with OSA requires a new formula of skeletal development for both maxilla and mandible based on correction of the immediate medical problem evaluated by overnight sleep testing called polysomnography (PSG) (attended) or home sleep testing (HST) (unattended).
This article seeks to evaluate the 3D volumetric changes that are necessary to treat pediatric Obstructive Sleep Apnea (OSA). Adult static therapies are not indicated for children. Children require dynamic therapies to encourage and correct skeletal development to improve sleep-breathing disorders. Formulas for arch width expansion are currently based on dental space and skeletal calculations and are not applicable nor are they validated in the treatment of pediatric OSA. Treating children with OSA requires a new formula of skeletal development for both maxilla and mandible based on correction of the immediate medical problem evaluated by overnight sleep testing called polysomnography (PSG) (attended) or home sleep testing (HST) (unattended).
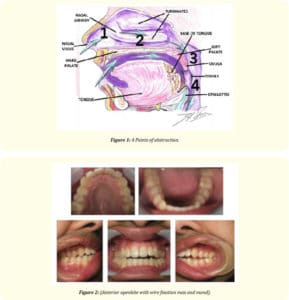
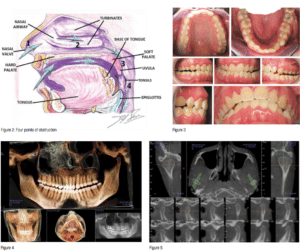
 Optimal is a very different than acceptable, especially if you are the patient. This case study will highlight the need for a structural assessment of the 4 points of the airway prior to treatment utilizing CBCT (i-CAT). In additional, this case report will demonstrate how successful resolution of sever apnea with an oral appliance on a patient for whom continuous positive airway pressure (CPAP) had little effect on excessive fatigue until the nasal airway was addressed.
Optimal is a very different than acceptable, especially if you are the patient. This case study will highlight the need for a structural assessment of the 4 points of the airway prior to treatment utilizing CBCT (i-CAT). In additional, this case report will demonstrate how successful resolution of sever apnea with an oral appliance on a patient for whom continuous positive airway pressure (CPAP) had little effect on excessive fatigue until the nasal airway was addressed.
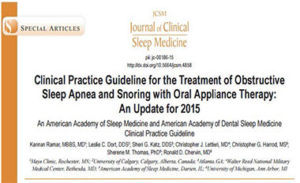 Introduction Since the previous parameter and review paper publication on oral appliances (OAs) in 2006, the relevant scientific literature has grown considerably, particularly in relation to clinical outcomes. The purpose of this new guideline is to replace the previous and update recommendations for the use of OAs in the treatment of obstructive sleep apnea (OSA) and snoring. Methods The American Academy of Sleep Medicine (AASM) and American Academy of Dental Sleep Medicine (AADSM) commissioned a seven-member task force. A systematic review of the literature was performed and a modified Grading of Recommendations Assessment, Development, and Evaluation (GRADE) process was used to assess the quality of evidence. The task force developed recommendations and assigned strengths based on the quality of the evidence counterbalanced by an assessment of the relative benefit of the treatment versus the potential harms. The AASM and AADSM Board of Directors approved the final guideline recommendations.
Introduction Since the previous parameter and review paper publication on oral appliances (OAs) in 2006, the relevant scientific literature has grown considerably, particularly in relation to clinical outcomes. The purpose of this new guideline is to replace the previous and update recommendations for the use of OAs in the treatment of obstructive sleep apnea (OSA) and snoring. Methods The American Academy of Sleep Medicine (AASM) and American Academy of Dental Sleep Medicine (AADSM) commissioned a seven-member task force. A systematic review of the literature was performed and a modified Grading of Recommendations Assessment, Development, and Evaluation (GRADE) process was used to assess the quality of evidence. The task force developed recommendations and assigned strengths based on the quality of the evidence counterbalanced by an assessment of the relative benefit of the treatment versus the potential harms. The AASM and AADSM Board of Directors approved the final guideline recommendations.
 by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO I am so excited to be a dentist in the year 2014. I started out way back in 1977 as a freshman at the University of Southern California dental school wanting to help people by relieving their pain and preventing them from having it. As my practice evolved from giving relief from dental, bony and soft tissue infections, inflammation and injuries to the relief of Craniofacial Pain and Sleep Breathing Disorders, I am impressed. I am impressed and proud that we have a profession that is so expansive in its’ ability to help people that we can limit our services to addressing medical conditions as a Dentist
by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO I am so excited to be a dentist in the year 2014. I started out way back in 1977 as a freshman at the University of Southern California dental school wanting to help people by relieving their pain and preventing them from having it. As my practice evolved from giving relief from dental, bony and soft tissue infections, inflammation and injuries to the relief of Craniofacial Pain and Sleep Breathing Disorders, I am impressed. I am impressed and proud that we have a profession that is so expansive in its’ ability to help people that we can limit our services to addressing medical conditions as a Dentist
 by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO We need to evaluate our system of treatment. A patient presents with worn dentition or complaints of muscle soreness. The dentist produces a nightguard without further in vestigation. The result is that the treatment helps the symptom of muscle soreness, makes it worse or has no effect. The dentist is unclear what to do.
by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO We need to evaluate our system of treatment. A patient presents with worn dentition or complaints of muscle soreness. The dentist produces a nightguard without further in vestigation. The result is that the treatment helps the symptom of muscle soreness, makes it worse or has no effect. The dentist is unclear what to do.
 © Springer-Verlag 2007 Patients with temporomandibular dysfunction (TMD) require correction of mandibular position, but the ideal position for the mandible remains controversial. Miralles et al. [1] found the amount of freeway space (FS) required depended on the protocol used to measure it. For example, a significantly higher clinical FS value was found using a phonetic method than after swallowing or with the mandible in a relaxed postural position. A sibilant is the hissing or whistling sound heard in the formation of certain letters in speech, such as the letter “s.” A phoneme is the smallest unit of speech that defines one sound from another.
© Springer-Verlag 2007 Patients with temporomandibular dysfunction (TMD) require correction of mandibular position, but the ideal position for the mandible remains controversial. Miralles et al. [1] found the amount of freeway space (FS) required depended on the protocol used to measure it. For example, a significantly higher clinical FS value was found using a phonetic method than after swallowing or with the mandible in a relaxed postural position. A sibilant is the hissing or whistling sound heard in the formation of certain letters in speech, such as the letter “s.” A phoneme is the smallest unit of speech that defines one sound from another.
TMJ & Sleep Therapy Centre of Kansas City is affiliated to TMJ & Sleep Therapy Centre International with now over 60 centres in 7 countries that are practicing utilizing Dr. Olmos standardized practice parameters.
